22 February 2019
 What do self-driving cars, solar airplanes and renewable energy have in common with the human heart? At first thought, not a great deal, yet a recent scientific endeavour called the Living Heart Project has brought together experts in engineering, aeronautics and energy to produce a sophisticated new model of the human heart for use in medical research. This 21st century approach to understanding heart disease is vitally important and of particular relevance in February – American Heart Month. Heart failure is a serious problem affecting 26 million people worldwide; heart disease causes 1 in 4 deaths annually in America. It can occur at any age, but becomes more common as we get older. Plus, different forms of heart failure affect men and women differently and require different treatments.
What do self-driving cars, solar airplanes and renewable energy have in common with the human heart? At first thought, not a great deal, yet a recent scientific endeavour called the Living Heart Project has brought together experts in engineering, aeronautics and energy to produce a sophisticated new model of the human heart for use in medical research. This 21st century approach to understanding heart disease is vitally important and of particular relevance in February – American Heart Month. Heart failure is a serious problem affecting 26 million people worldwide; heart disease causes 1 in 4 deaths annually in America. It can occur at any age, but becomes more common as we get older. Plus, different forms of heart failure affect men and women differently and require different treatments.
Efforts like the Living Heart Project are long overdue, survival rates for heart failure patients have not improved since the 1990s. Despite a half-century of research funding and countless rodent experiments, translation of animal data to people has been poor to non-existent. Not surprising perhaps, considering the differences in size and development, heart rates, oxygen consumption, contractility, protein expression, and stem cell populations between humans and rodents. Calls for ‘improved animal models’ for human heart disease favored larger animals – such as dogs – due to closer resemblance of cardiac physiology between dogs and humans (compared to rats and humans). Experimental induction of heart failure in the young, healthy dogs employed as models is severe – often requiring complex, extensive surgery – and distressing. In addition to these ethical concerns, there are scientific reasons to move away from canine models of heart failure – the collateral coronary circulation in dogs creates inconsistency and heterogeneity in the response to myocardial lesions which make comparison of post-injury outcomes difficult.
In people, kidney disease is often associated with heart disease: reduced kidney function increases the heart rate as more blood is pumped to the kidneys, which increases blood pressure and impacts the heart. To investigate the effects of high blood pressure in canine models of disease, dogs have their kidneys wrapped tightly to block blood flow and cause irreversible damage. In 2016, nine elderly dogs underwent this operation in a study to investigate tissue changes in the heart. This occurred despite earlier evidence of this so-called ’tissue remodelling’ in people with heart failure and the use of markers of tissue remodelling to diagnose heart failure in people. In 2015, the Living Heart Project showed that sophisticated computer models can predict the heart tissue changes that are seen in the clinic. This represents a major advance and further reduces justification for the animal experiments.
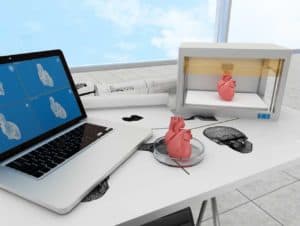
Other advances are also moving us away from reliance on animal models. In 2015, scientists from Massachusetts General Hospital and Harvard Medical School seeded human induced pluripotent stem cells (iPSC) into acellular scaffolds to produce a beating heart, with the ultimate aim of creating a perfect match for people in need of a heart transplant. At Stanford University Cardiovascular Institute, scientists are combining CRISPR/Cas9 with iPSC cultures of patient heart cells to create a personalized heart disease risk assessment platform – enabling assessment of possible pathogenic effects of different mutations. Scientists at the University of Tokyo, with Tokyo Women’s Medical University and RIKEN in Japan, have developed a flexible nanomesh sensor to monitor functional activity of cardiac models without interfering with cell function – allowing real-time assessment of drug response in a human-relevant model system.
Combining these exciting new technologies can further revolutionize research – the BioMed21 collaboration funded review Cardiovascular Disease Models: A Game Changing Paradigm in Drug Discovery and Screening proposes a new paradigm for research into cardiovascular diseases. This is rooted in a human-specific understanding of disease mechanisms, coupled with application of novel microphysiological and computational tools based on human biology to create more predictive laboratory models of the human disease.
It seems that there is much to celebrate in human-relevant heart research, and no need to break any more animal hearts.

Post a comment