19 July 2019
 This edition of research round-up reports on very different aspects of applying human-focused technologies and strategies. The paper by Velasco et al. entitled ”Individual brain organoids reproducibly form cell diversity of the human cerebral cortex” and published in Nature shows that results obtained from brain organoids are reliable and can be replicated. In their paper ”Phosphorylation of SOCS1 inhibits the SOCS1-p53 tumor suppressor axis” published in Cancer Research, Ferbeyre et al. unveil the molecular mechanisms that turn a tumor suppression gene into an oncogene and suggest that an FDA-approved drug may stop this oncogene. Lastly, the study “Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip” published in Nature Biomedical Engineering by Occhetta et al. reports on the development of a human cartilage-on-a-chip to be used for screening new drugs for Osteoarthritis.
This edition of research round-up reports on very different aspects of applying human-focused technologies and strategies. The paper by Velasco et al. entitled ”Individual brain organoids reproducibly form cell diversity of the human cerebral cortex” and published in Nature shows that results obtained from brain organoids are reliable and can be replicated. In their paper ”Phosphorylation of SOCS1 inhibits the SOCS1-p53 tumor suppressor axis” published in Cancer Research, Ferbeyre et al. unveil the molecular mechanisms that turn a tumor suppression gene into an oncogene and suggest that an FDA-approved drug may stop this oncogene. Lastly, the study “Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip” published in Nature Biomedical Engineering by Occhetta et al. reports on the development of a human cartilage-on-a-chip to be used for screening new drugs for Osteoarthritis.
Reliable 3D brain organoids
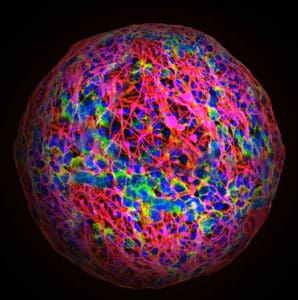
Embryonic brain development is essentially the same for every one of us- the same regions are formed, made up of the same cell types carrying out the same functions. Models of the human brain have been under development for many years, with increasing sophistication, such that we are now accustomed to reading about three dimensional, multi-cellular organoids and spheroids that exhibit increasing developmental maturity – but creating different models in different labs with different protocols has issues of its own. Besides the fact that animal data is not translatable to humans and that animals are poor models for human diseases, there is a reproducibility crisis in animal research – and research employing purely in vitro methods may not be far behind. For models that employ induced pluripotent stem cells (iPSC), it is crucial that researchers fully describe the differentiation protocol adopted – to ensure confidence in the cell type under test but also to permit the rigorous replicate studies that are necessary to advance the research. It is therefore promising to see that Velasco et al., in their paper ‘Individual brain organoids reproducibly form cell diversity of the human cerebral cortex’ published June 5 in Nature have established protocols for producing 3D organoid cultures, using five different human stem cell lines.
Using defined culture methods to reduce hypoxia in order to create three- and six-month old organoids, the authors then carried out single-cell RNA-sequencing, extracting RNA from a total of 166,242 cells from eleven individual organoids. This analysis revealed that the cellular composition of the cultures was highly reproducible in terms of cell identity and cell diversity. In addition, immunohistochemistry analysis of neuronal markers indicated that development of organoids continued over time, with 6-month cultures containing appropriate, additional cell types.
The authors note that the use of stem-cell based models of the brain in the investigation of human brain development has been limited by several factors, not least of which is the issue of organoid reproducibility. This latest research demonstrates several key features that could improve application of stem cell models:
1. Generation of cellular diversity can, and does, occur outside of the embryonic environment
2. Development of cellular diversity is highly reproducible
3. Early patterning of brain development can be maintained outside the embryonic environment
Overall, the important contribution of this research is in the demonstration that human brain organoids can model the dynamic processes of human brain development in a reproducible manner – leading to the authors final conclusion that these cultures “establish[es] a valuable organoid model amenable to the experimental investigation of developmental abnormalities associated with human neurological disease.”
Promising new FDA-approved drugs for treating lymphoma
Cancer is a disease of the molecular regulatory system. When molecules do not play their roles according to the plan, cells go astray and may never die. A big challenge in cancer research is to discover the role playing by specific molecules, with the additional complication that these roles may change depending on the environment and behavior of other surrounding molecules. Cancer is a complex system of many moving pieces that orchestrate their functions in a species-specific manner. To unveil the regulation and roles of molecules in human cancer, the research needs to look into human systems.
One of the moving pieces in cancer development that has attracted great attention is the suppressor of cytokine signaling-1 (SOCS1), a molecule that is overexpressed in some cancers while in others is inactivated. When normally expressed, SOCS1 works with p53 and together the two suppress the formation and progression of tumors.
However, melanoma and colorectal cancer seem to be the result of an overexpressed SOCS1 that has acquired oncogenic proprieties, while in solid cancers SOCS1 is often inactivated. To understand how the same molecule can show contrasting roles, Gerardo Ferbeyre at the Université de Montréal and the CRCHUM, in Canada, led a group that investigated the interaction between SOCS1 and p53 by studying cell lines from lymphoma patients carrying mutations at the SOCS1 motif called Y80. It is through this motif that p53 interacts with SOCS1.
The authors of the study “Phosphorylation of SOCS1 inhibits the SOCS1-p53 tumor suppressor axis”, published in the journal Cancer Research in May 2019, found that cells carrying specific mutations at the SOCS1 Y80 motif have this site permanently phosphorylated and as such the molecule loses its ability to bind to p53 and fails to inhibit cell proliferation, acquiring oncogenic proprieties.
An important implication of this finding for patients carrying a mutated SOCS1 at the Y80 motif is that they do not respond to doxorubicin, a common drug found in chemotherapy regimens. On the other hand, the authors of the study found that the phosphorylation of the mutated SOCS1 is carried out by the SRC family of tyrosine-protein kinases, a class of molecules for which a number of inhibitors are currently being used to treat a variety of cancers. In this study, the authors treated mutated cells with dasatinib, a tyrosine-kinase receptor inhibitor, and were able to restore the SOCS1-p53 axis and its tumor suppressing proprieties. For cell lines in which both p53 and SOCS1 are mutated, the study shows that treating p53 with PRIMA-1, a compound that reactivates p53, followed by treating the cells with dasatinib also restore the SOCS1-p53 axis and its anti-proliferative function.
Considering that SRC inhibitors are FDA-approved for cancer treatment, these findings offer new hope for patients carrying mutations in the SOCS1 gene and for those with high levels of phosphorylated SOCS1 and who have failed to respond to common chemotherapy treatments.
An efficient cartilage-on-a-chip for screening disease-modifying osteoarthritic drugs
Osteoarthritis (OA) is an age-related musculoskeletal disease and the fifth leading cause of disability worldwide. It is characterized by a whole-joint pathological active response to environmental factors such as abnormal mechanical loading and oxidative stress. These are associated with the onset of inflammation, resulting in cartilage degeneration and alterations of subchondral bone, synovium and ligaments. None of the treatments available for OA can reverse the disease but only mitigate patient symptoms. Disease progression can be reduced by disease-modifying osteoarthritic (DMOA) drugs, but these are scarce mainly because of lack of relevant pre-clinical OA models. In addition to differences in anatomy and physiology between humans and animals, which make animals an imperfect model for studying interventional methods, animal models are also costly and time-consuming, making in-vitro models of the disease a highly desirable option. Thus, in vitro models that can reliably predict the efficacy of DMOA drugs are the need of the hour.
3D macroscale systems that integrate cells, soluble factors, and extracellular matrix-like matrices have been used to model articular cartilage, aiming to recapitulate both cellular-specific architecture and the mechanical environment. However, the generation of such engineered cartilage constructs requires bulky and complex bioreactor systems, thus preventing their widespread use as in vitro models. Current in vitro models rely either on biochemical (cytokine-based) or mechanical (load-based) stimulation.In their paper, ‘Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip’ published June 3rd in Nature Biomedical Engineering, Paola Occhetta et al., reported the development of a microscale system that can reproducibly generate a human cartilage-on-a-chip (COC). This was achieved by integrating a polyethylene glycol hydrogel-based 3D microenvironment and a mechanical actuation system able to provide defined levels of confined compression. By recapitulating the mechanical stimuli involved in OA pathogenesis, and applying compression as a main component of cartilage deformation, OA traits were induced in COC. A total of 30% of confined compression recapitulated the mechanical factors that are involved in OA pathogenesis. The hyperphysiological compression triggered a shift in the cartilage homeostasis towards catabolism and inflammation, hypertrophy, and acquisition of gene expression profile, which was comparable to what is seen in the clinical OA tissue. The scientists used anti-inflammatory and anti-degrading drugs that were clinically approved, or under development, with the osteoarthritic COC model, showing its potential to work as an effective preclinical tool for testing new DMOA candidates in a predictive fashion. Thus, COC can be used for the screening of DMOA candidates.
This research overcomes the barriers encountered by current in-vitro models that rely either on cytokine-based stimulations, which hampers recapitulating the OA environment that is found in vivo, or on load-based stimulations that are unable to fine-tune the stimuli provided to the tissue, and thus fail in reproducing the environment of the native joint physiology and/or pathology.
The authors concluded that achieving a dense matrix rich in cartilage extracellular matrix components, together with a gene expression that is similar to the type found in native chondrocytes, made the COC model functionally responsive. The system presented in the study allows for achieving COC models in a highly reproducible manner, which was tested with donor samples from five different human donors, thus countering the reported high donor-to-donor variability of primary human articular chondrocytes.

Post a comment