5 November 2019
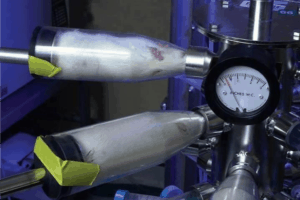
Rats jammed face first into what look like small milk bottles, no room to move, no option to even turn their heads. The rats in glass cylinders are arranged rows deep, screwed into a huge central metal cylinder that will provide a constant stream of cigarette smoke, directed into their faces in what is known as the ‘nose-only’ exposure technique. Mice contained in small plastic boxes for hours on end, flooded with a constant stream of cigarette smoke at a rate of 10 cigarettes per hour, with no break. This is the ‘whole body’ exposure model. Dogs trapped, immobilised, their noses strapped into masks, their eyes just visible peeking above. Or how about mice, with patches shaved on their backs, cigarette tar painted onto the bare skin until tumours appear? Tobacco distillate rubbed into a rabbit’s skin? The toxic compounds we now associate with smoking-related disease fed to rats until they develop fatal oesophageal tumours? These approaches have all been used to examine the effects of cigarettes, and shockingly, many are still used today.
Experiments rubbing concentrated cigarette smoke extracts into animal skin were carried out for many years in attempts to discover whether cigarettes were harmful. Careers were made or destroyed here; the scientists using strains of mice that did not get cancer received further funding to continue down an essentially blind alley, whilst the researchers using animal models which showed that smoking could cause cancer were not funded again. I think that we are probably all aware of this back story; tobacco companies accused of not revealing all their data indicating that cigarettes were really harmful, and groups like the Guest Choice Network (now Center for Consumer Freedom), who were paid to try and stop smoking bans, but part of the issue here was that cigarettes were really not that harmful… if you were a rat or a mouse. This is still a huge problem with research using animals; animal models do not mimic the severity of (smoking-related lung) disease as we see it in people. However, for people, smoking really is bad for you! Around 90% of people who smoke will develop Chronic Obstructive Pulmonary Disease or COPD. COPD is a progressive lung disease, and consists of chronic obstructive bronchiolitis, emphysema and mucus plugging. This means that people with COPD experience obstruction of their airways, destruction of lung tissue and loss of lung elasticity; all making it really hard to breathe. There are many different cell types and mechanisms involved in COPD and the disease progresses over time from stage 0 (people at risk of COPD but not yet diagnosed) to stage 4 (very severe).
Fundamental differences in basic anatomy, as well as how animals breathe (rodents are obligate nose-breathers), makes it hard to see how smoking animal models could ever relate to the human lung disease. The complexity of COPD, the fact that it is not one condition, means that no single animal model models the entire disease. Researchers using animal models may “pick-and-mix” different elements, for example, using genetically modified mice, deliberately infecting mice with viruses or bacteria, or instilling damaging proteolytic enzymes into the lungs before exposing the animals to cigarette smoke. Trying to piece together results from a range of animal models, instead of investigating a more complete disease system, has led to many failed clinical trials and a failure to provide much-needed therapies. Enzyme inhibitors designed to reduce lung damage that were successfully tested in mice showed no improvement in people after 3 months. Another compound designed to reduce lung inflammation gave people side effects (headaches and nausea) and still did not improve their lung function. So, drugs that have shown “promise” in the horribly engineered and fake animal models have, at best, resulted in no improvement for people with COPD.
So are we back where we started, with limited new drugs in the development pipeline? Over 80% of active clinical trials for people with COPD focus on behavioural and dietary interventions or designs of new medical devices for existing treatments.
Thankfully, as we move into Global COPD awareness month there are many reasons to be cheerful, if you are a human, or a mouse…. New techniques have the potential to reveal new treatments to reduce the lung damage typical of COPD and do not use mice, or rats, or dogs. An exciting report published recently indicates how advanced cell culture techniques can vastly improve our ability to understand and treat COPD. Whilst we have had access to three-dimensional tissue culture models of the human airways for some time, this recent study has added a further dimension; it can breathe! The model is made up of human lung cells, grown on a tiny silicon chip and it can be made to inhale cigarette smoke with the same puff duration, puff intensity and puffs per cigarette as a human smoker. Results from these microphysiological systems indicate that healthy airways respond as expected, with increased signs of inflammation and damage after smoke exposure. This is exciting, but not the most important feature of the models. What we really need to be thrilled about is that this in vitro model can be ‘built’ using airway epithelial cells from people with COPD. So now we can use a human-predictive, physiologically relevant system to examine whether experimental new drug treatments will be effective for COPD, and we can keep the rats away from the milk bottles, unless they are thirsty!

Post a comment