24 May 2022
 by Bianca Marigliani
by Bianca Marigliani
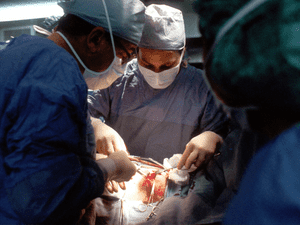
Current patients’ need for organ transplantation far exceeds the availability of donors [1]. This is a pressing issue with a distressing human cost: all over the world people die while still on the waiting list for donated organs. To address this issue and save lives, some scientists have proposed xenotransplantation as a solution for the worldwide organ shortage crisis and recent press reports have discussed breakthroughs with this technique.
The first successful heart transplant from a genetically modified pig to a human being hit the headlines in January [2]. The 57-year-old patient, who had advanced heart failure, received a pig’s heart with ten genetic modifications. These included knock out of certain pig genes and the addition of human genes to reduce the risks of rejection, as well as removal of a growth hormone receptor gene to reduce the growth of pig heart tissue after transplantation. Sadly, the patient died in March 2022.
January 2022 also saw the University of Alabama at Birmingham’s announcement concerning the transplant of genetically modified pig kidneys into a neomort, a brain-dead human, after performing a prospective histocompatibility test. The transplanted kidneys remained viable until the end of the study, which lasted three days. Despite the development of progressive multisystem organ failure and no creatinine clearance recovery, the study’s authors claim to have overcome the major difficulties of human xenotransplantation and identified areas for additional research and clarification [3].
In both instances no hyperacute rejection was observed. According to the researchers, this was achieved by using CRISPR-Cas9 genome editing, and so these cases represent the latest development in combining gene editing with xenotransplantation. However, neither the hurdle of chronic rejection of xenotransplants, nor the potential of cross-species infection and diseases transmission, a concern frequently raised in the context of this technique, have been overcome. In fact, recent reports indicate that a porcine virus may have contributed to the death of the patient who received a gene-edited pig heart [4]. Many human viruses are suspected to have originated in animals, so xenotransplantation may put not only the patient who receives the organ in peril but the procedure could put the whole society at risk [5].
The treatment and fate of the pigs raised in specialized facilities used to make xenotransplantation possible also raise animal welfare concerns [6]. Nonetheless the proponents of this approach believe that, in the future, it could be used systematically for patients suffering from diseases such as diabetes, heart diseases, kidney failure and Parkinson’s disease.
It should be said, however, that the emergence of other scientific and technical approaches, beyond the reservations already described, raises doubts as to whether or not xenotransplantation is the best hope for patients and the best choice for society.
Human heart transplantation has been the standard therapy for terminal heart failure. A clinical trial for a total artificial heart aims to provide a lasting solution for this disease. This new-generation artificial heart is approved for use in Europe, and the first successful implantation in the U.S. was reported in July 2021 [8].
Techniques such as bioprinting and biofabrication of human tissues hold great promise for engineering-based organ replacement [9]. Current bioprinting technologies focus to a large degree on producing transplantable tissue, e.g. cardiac patches for the repair of damaged myocardium. Personalized bioprinting approaches have already been used to develop heart valves to replace defective ones in patients. By using patient-specific materials, bioprinting has the potential to produce translatable artificial organs. Although many bioprinting and biofabrication technologies use animal components such as fetal bovine serum, Matrigel and gelatin, “clean bioprinting”, an approach devoid of animal components, has been gaining ground [10].
Recent advances in embedded 3D bioprinting, such as the freeform reversible embedding of suspended hydrogels (FRESH), are revolutionizing the fabrication of geometrically complex biomaterials. The application of such technology is making it possible to achieve high print fidelity while mimicking the elasticity of tissues and structures. This represents a promising strategy for overcoming one of the key barriers to fabricating functional adult-sized tissues and organs [11]. Although we are still a long way from being able to print whole human organs for transplantation, the continuing pace of breakthroughs in this field provides strong incentive for research funding agencies to make significant investments in 3D bioprinting.
Another avenue toward resolving our organ shortage is to increase organ donations through targeted policies and incentives. The EU Action Plan on Organ Donation implemented from 2009 to 2015, for example, increased donations by 21% during that period [12]. There is plenty of room to improve on these figures when we take account of the differential rates of organ donations between countries, which varies from 1.7 donors per million population in Cyprus to 48.3 donors per million in Spain [13].
A successful response to the chronic deficit of available organs for patients who need them will require intelligent public health policies and strategic investment approaches. It is not clear that animal organ transplants can effectively meet the demands of the situation. For that reason, we should encourage governments, medical institutions and other stakeholders to pursue dynamic social marketing initiatives to boost organ donor commitments. We should also take stock of the remarkable emerging advances in biomedical research that promise to displace animal organ transplants on their merits, and take advantage of their potential as a more efficient path to address organ shortages. These lines of advance may do more for patients, and for society, in the longer run.
What do you think? Please share your thoughts and comments below.

Post a comment