13 October 2020
 by Marcia Triunfol
by Marcia Triunfol
This week, the founding director of The Wyss Institute for Biologically Inspired Engineering at Harvard University, Dr Donald Ingber, questioned journal editors and peer reviewers about a new form of publication bias. In an opinion piece in Advanced Science entitled, “Is it Time for Reviewer 3 to Request Human Organ Chip Experiments Instead of Animal Validation Studies?,” Ingber questions why animal data is still considered the gold standard in human health research, while presenting evidence that organs-on-chips (organs chips) may better suit this purpose.
A recent success story for human organ chip technology involves a rare genetic disorder called Shwachman-Diamond Syndrome (SDS). SDS affects the bone marrow of one in every 80,000 newborns, rendering patients vulnerable to infections due to low neutrophil counts. Animal models, from mice to zebrafish, have failed to provide meaningful insights. However, Ingber at the Wyss Institute, and collaborators, built an SDS Bone Marrow chip (BM chip) using neutrophil progenitor cells isolated from the bone marrow from SDS patients. This work provided the crucial insight that the main impairment in SDS is in the maturation process of CD34+ hematopoietic progenitor cells, opening new opportunities for drug discovery.
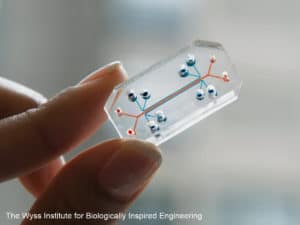
Many drugs can have a toxic effect on the bone-marrow, so developing a system that could predict drug-induced toxicity in patients would be of great value. In the same study, the group also shows that the BM chip made it possible to replicate human drug exposure profiles, such as drug pharmacokinetics, previously measured in patient blood samples. Predicting drug pharmacokinetics is one of the main reasons drugs tested in animals fail in clinical trials. The BM chip is one of several organ chip microfluidic culture devices developed in recent years.
There are other breakthroughs attributed to human organs chips. The Lung Alveolus Chip showed that physiological breathing motion, not the presence of immune cells, is the main reason cancer patients develop edema when treated with IL-2 and that the pharmacological agent GSK2193874, which blocks the TRPV4 ion channel activated by mechanical strain, can prevent it. Other TRPV4 inhibitors have been tested in clinical trials as potential therapeutics for improving pulmonary function. A more recent version of the Lung Alveolus Chip helped to elucidate how bacterial lipopolysaccharide endotoxin stimulates intravascular thrombosis. Currently, Human Lung Airway Chips are being used to study infection by SARS-CoV-2 and to test FDA-approved drugs as potential candidates for treating COVID-19.
Besides working with a single chip, multiple organ chips can be linked together by transferring fluid among their vascular channels to create a human body on chips. With a multiple organ chip that included gut, liver and kidney chips, Ingber and collaborators were able to follow the absorption, metabolism and excretion steps that a drug undergoes in the body and quantitatively predict drug pharmacokinetics in humans.
These are just few of the examples of how organs-on-chips can shed light on the underlying mechanisms of human diseases and facilitate drug development and translate the findings obtained in the lab into real benefits for patients. As an added benefit, organs on chips allow patients’ cells to be used and tested directly, an important step towards personalized medicine.
Ingber notes that some editors of scientific journals and/or peer-reviewers continue to regard animal model data as the gold standard, including making acceptance for publication conditional on providing “proof in animals,” which may involve performing new animal experiments to generate in vivo data. We asked Ingber if he has ever been required by journal editors or peer reviewers to include or produce new animal data in a study that was originally submitted without using animals, and whether this was a condition for the paper to be accepted. “Yes,” he replied, “Multiple times, and we had to obtain new data to get our first breakthrough article on organ chips published (Lung Chip paper in Science in 2010). The worst case was my paper on lung cancer-on-a-chip, where we found breathing motions regulate cancer growth, and the reviewer demanded that we confirm this in mice. It was only when I called the editor and explained that I can’t keep mice alive for the 3-week tumor growth experiment when not breathing that they allowed me to bypass this request.”
Ingber is frustrated with the difficulties in having human organs chips data fully accepted in their own right, particularly when it is known that animal models do not effectively mimic human responses. For instance, animal data are still required by regulatory agencies, such as the U.S. Food and Drug Administration and European Medicines Agency, in order for a drug to be approved for use in humans. Yet if results obtained with animal models are significantly different than those obtained with a human organs chips, which do we trust? “We have to use animals because our funding agencies require it,” said Ingber, but “for cases involving repurposing of FDA approved drugs where we know the pharmacokinetics (PK) in humans, we would like to do a thorough analysis to show that we can fully recapitulate dynamic human PK results in other organ chips. Thus, if under these conditions, we get potent inhibition of viral infection with a drug that does not work in animals, I would still hope that regulatory agencies might take this into account, or that drug companies might take the chance to move it into clinical trials. But this is easier said than done.”
Ingber also laments that “nobody wants to take the risk of changing the way they do things,” and “most labs will do what they have always done, and the benchmark is the mouse model.”
So, what can be done to tackle bias in journal peer review and editorial policy to support scientists adopting the use of models other than animals? Ingber believes that “we need to use replication of human clinical data as a benchmark for publications, and when it comes to drugs, we need to do this while recapitulating clinically relevant PK on-chip. If this can be demonstrated on-chip, then it is definitely better than mice.”
Now we, at Humane Society International, ask: does it ever make scientific or ethical sense to require that animal data be produced to “validate” results obtained with a more advanced human-focused technology that better emulates human biology, as a condition for paper acceptance? This is a timely question in urgent need of a sound answer.
What do you think? Please share your thoughts and comments below.

A says
Mice, rats, birds and other species used in science/research/education are not counted because they have been deliberately excluded from the definition of “animal” in the Animal Welfare Act.
These animals are invisible. They are massacred with impunity. In laboratories. By educated people who are either indifferent to their suffering or powerless to stop it.
However… living, breathing beings have the right not to be subjected to experiments, confinement, isolation, pain or deprivation. They have inherent rights and deserve to be protected under the law.
So, no matter how “useful” animal models are or how commendable the endeavors to find cures for humans, regulatory agencies should be forced to rely only on effective, ETHICAL, NON-ANIMAL methods and models.
First Do No Harm
There is No Excuse for Abuse
All Animals Have the Inherent Right to Be Counted and to Be Treated with Dignity and Respect
Animals are Individuals and Need to be Granted Personhood
Science is advancing with the development of non-animal alternatives
Regulatory agencies that require (or even consider) animal models are still in the Dark Ages
Please develop, use and accept only non-animal alternatives/models/methods
Please update all regulatory requirements by eliminating any mention, requirement or option of animal use
No individual of any species (vertebrate, invertebrate or other) should ever be used in the name of “science,” “progress” or “humans.”
No More Animal Sacrifices
Advance Science
End Speciesism
Lindsay Marshall says
It is a concern that there is a continued requirement for animal data from journal reviewers/editors, with the underpinning message that these data are somehow ‘better’ or more relevant than the data from human cell-based chips (or other non-animal methods). This is surely damaging scientific progress and hindering the uptake of chip data (in place of animal data) by regulatory agencies.
We are exploring how to prevent this in order to encourage the acceptance and publication of in vitro data as gold standards in their own right.
During the peer review process, has this request for animal data as an add-on to a purely in vitro study happened to you and would you share your story with us? You can contact us on admin@biomed21.org Thanks!