13 December 2018
 Diabetes treatment is often touted as the poster-child success of animal research; after all, insulin was first discovered in dog pancreas almost 100 years ago. A lot has changed since then. Or at least it should have. The reality is that billions of research dollars are still wasted on ineffective animal models of diabetes that are not translating to therapies delivering effective glycaemic control for patients. For instance, oral insulin and nicotinamide were both therapeutic interventions that showed promise in animals but failed in humans. A new review – ‘Future Roadmaps for Precision Medicine Applied to Diabetes: Rising to the Challenge of Heterogeneity’ – from clinical experts and published in the Journal of Diabetes Research, reveals the gap between animal models of diabetes and the human condition and calls for alternative, non-animal approaches to drive advances in research that are ‘clinically translatable’ and that apply existing and evolving methods of relevance to human focused research.
Diabetes treatment is often touted as the poster-child success of animal research; after all, insulin was first discovered in dog pancreas almost 100 years ago. A lot has changed since then. Or at least it should have. The reality is that billions of research dollars are still wasted on ineffective animal models of diabetes that are not translating to therapies delivering effective glycaemic control for patients. For instance, oral insulin and nicotinamide were both therapeutic interventions that showed promise in animals but failed in humans. A new review – ‘Future Roadmaps for Precision Medicine Applied to Diabetes: Rising to the Challenge of Heterogeneity’ – from clinical experts and published in the Journal of Diabetes Research, reveals the gap between animal models of diabetes and the human condition and calls for alternative, non-animal approaches to drive advances in research that are ‘clinically translatable’ and that apply existing and evolving methods of relevance to human focused research.
The crude experimentation with dogs in the 1920s provided us with a basic understanding of diabetes and it is clear that animals can only ever provide an incomplete understanding of disease. Research questions now are too complex to be answered by a model that superficially resembles the human condition; only human-focused models can answer the in-depth sophisticated questions that our improved understanding of disease have allowed us to formulate, and the explosion in biotechnology and the ‘omics revolution that have occurred in recent years are providing the human relevant tools to enable this. Shifting focus towards human studies has helped to reveal that diabetes is a multifactorial, heterogeneous spectrum of metabolic disorders with environmental and genetic elements, but it seems that a continued reliance on animal models has failed to provide a detailed understanding of disease pathogenesis or provide the elusive cures. [Read more…]
 Thrombosis-on-a-chip, vasculature-on-a-chip and engineered models of human cardiac fibrosis are just a few of the new technologies revolutionizing research into human cardiovascular disease—a condition responsible for 17 million deaths per annum globally. A new study entitled
Thrombosis-on-a-chip, vasculature-on-a-chip and engineered models of human cardiac fibrosis are just a few of the new technologies revolutionizing research into human cardiovascular disease—a condition responsible for 17 million deaths per annum globally. A new study entitled 
 Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection and a major public health concern, particularly for the very young and very old. Around the world,
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection and a major public health concern, particularly for the very young and very old. Around the world, 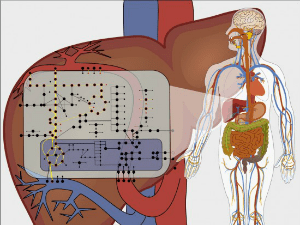 A
A 